Introduction – What is Leptin?
When most people in the health and fitness industry think about hormones, they think about how thyroid influences our energy expenditure, or how testosterone can shunt more of our calories to building muscle instead of putting on fat. It’s not that these hormones arent important; they certainly are, its just that those, along with insulin and other female sex hormones get the lion’s share of attention in the world of endocrinology.
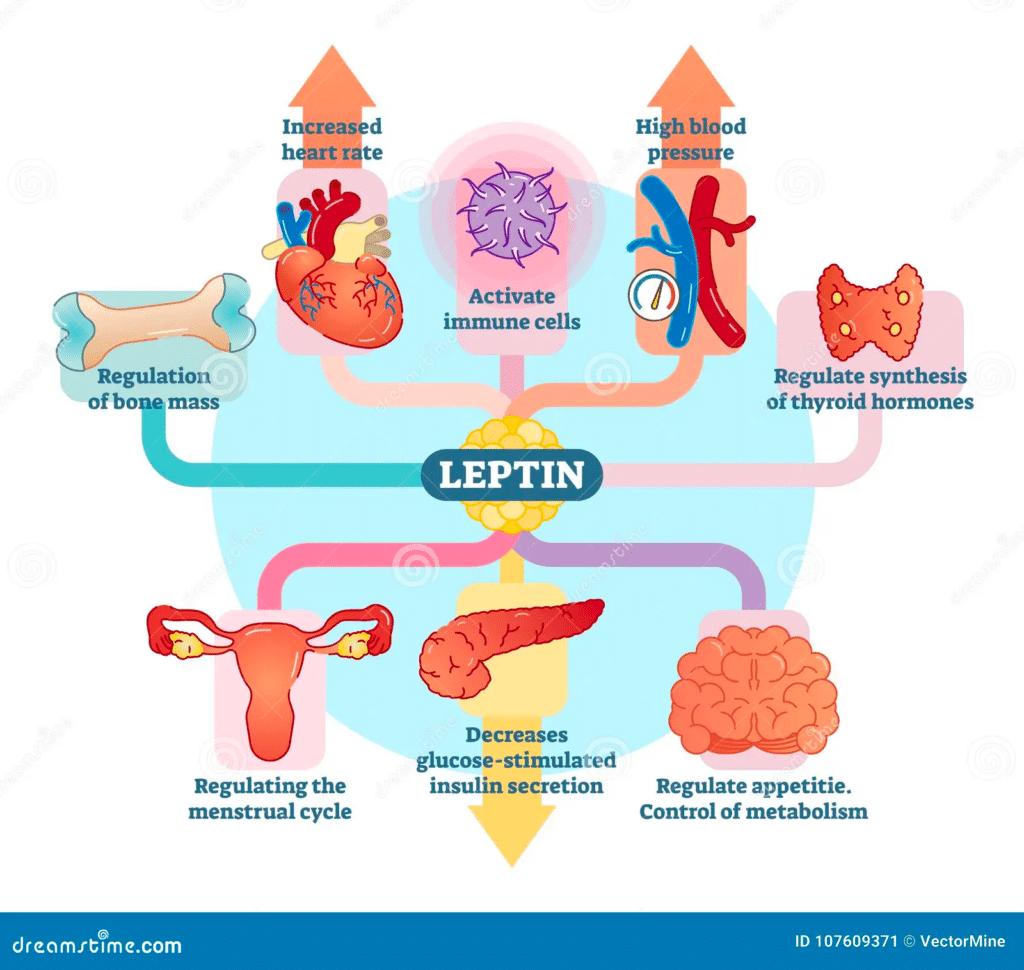
Enter leptin: One of the more recently discovered hormones in 1994, leptin is secreted from adipose tissue and regulates energy homeostasis, neuroendocrine function, metabolism, immune function and other systems through its effects on the central nervous system and peripheral tissues. In fact, the hormones we talked about just a bit ago, thyroid hormone and our sex hormones, are under direct control of leptin.
At a basic level, adipose tissue secretes leptin, and the more adipose tissue we have, the more leptin we’re secreting. It’s a long term satiety hormone that’s also in control of energy balance, meaning that more leptin should make us less hungry overall and increase energy expenditure, and less leptin should drive up appetite and decrease energy expenditure.
Leptin abnormalities have associations with a variety of health issues, particularly obesity, thyroid issues, sex hormone issues, metabolic syndrome, and resistance to fat loss. Leptin administration has been shown to restore metabolic and neuroendocrine abnormalities in individuals with leptin-deficient states, including hypothalamic amenorrhea and lipoatrophy. In contrast, obese individuals are resistant to leptin.
Why Care about Leptin? Low Leptin vs. Leptin resistance
In terms of body transformation, leptin is directly responsible for current energy expenditure levels as well as how hungry we generally are. Leptin is a master controller of other hormonal axis’, and low leptin levels lead to low thyroid and low sex hormone levels such as testosterone, estrogen, and progesterone, as well as IGF-1.
I talk a considerable amount about metabolic adaptation, or the process the body goes through to lower energy expenditure in response to low food intake. Low leptin is the top domino to fall within the physiological milieu of metabolic adaptation.
Those that are chronically dieting or very low body fat will inevitably have decreased leptin levels, which translates to lower energy expenditure directly from the low leptin, but also because of possibly having low thyroid levels as well. Combine that with the decreased testosterone and IGF-1, you also have much poorer nutrient partitioning with the calories you are consuming, leading to much less of an ability to put on or retain lean mass.
Leptin also interacts with cortisol, taking part in the expression of cortisol, so this is another piece of evidence that shows how it’s one of the first dominos responsible for the cascade of effects that occur during metabolic adaptation.
On the opposite end of the spectrum, most obese individuals experience leptin resistance, meaning their leptin is very high because of high levels of bodyfat, but they experience a resistance to the signal of leptin at the level of the brain.
This translates to all of the effects that we see in levels of low leptin, including decreased energy expenditure, increased hunger, and possibly leading to low thyroid, sex hormones, and IGF-1 as well.
Restoring proper leptin signaling would have a role in bringing numerous hormones back to homeostasis: contributing to reversing hypothalamic amenorrhea, or loss of cycle for women, restoring the ease of fat loss for those who are struggling, and more.
In the rest of the post, we’ll talk a little bit about the physiology of leptin and dive a little more into its roles and functions, talk a little about leptin disruptions in circadian disruption, as well as talk about what we might be able to do in states of low leptin and also leptin resistance.
Science of Leptin
Leptin is mainly produced by fat tissue, although present in many other tissues such as skeletal muscle, stomach, pituitary gland, and lymphoid tissue. In general, leptin levels reflect the amount of fat storage with higher circulating leptin levels correlating with higher fat tissue.
Leptin displays a circadian profile with lowest levels in the mid afternoon and highest levels around midnight (we’ll address more about the importance of the circadian aspect of leptin a little later). Obese individuals still display the rhythm, just at a higher level overall and higher peak in the night.
In addition to its roles in energy homeostasis and neuroendocrine (hormonal) function, it also plays a role in immune health as well.
Leptin Functions in Depth
Leptin’s Control of Body Weight through Hunger, Satiety, and Metabolism
Most people that know about leptin are familiar with one of it’s basic roles; its activity as a satiety signal. This action occurs within the brain, the hypothalamus specifically.
When leptin binds to its receptors in the hypothalamus, this has the effect of activating a set of neurons that decrease food intake and increase energy expenditure while also inhibiting neurons that do the opposite. Insulin also has this effect in insulin sensitive individuals. This can be seen below:
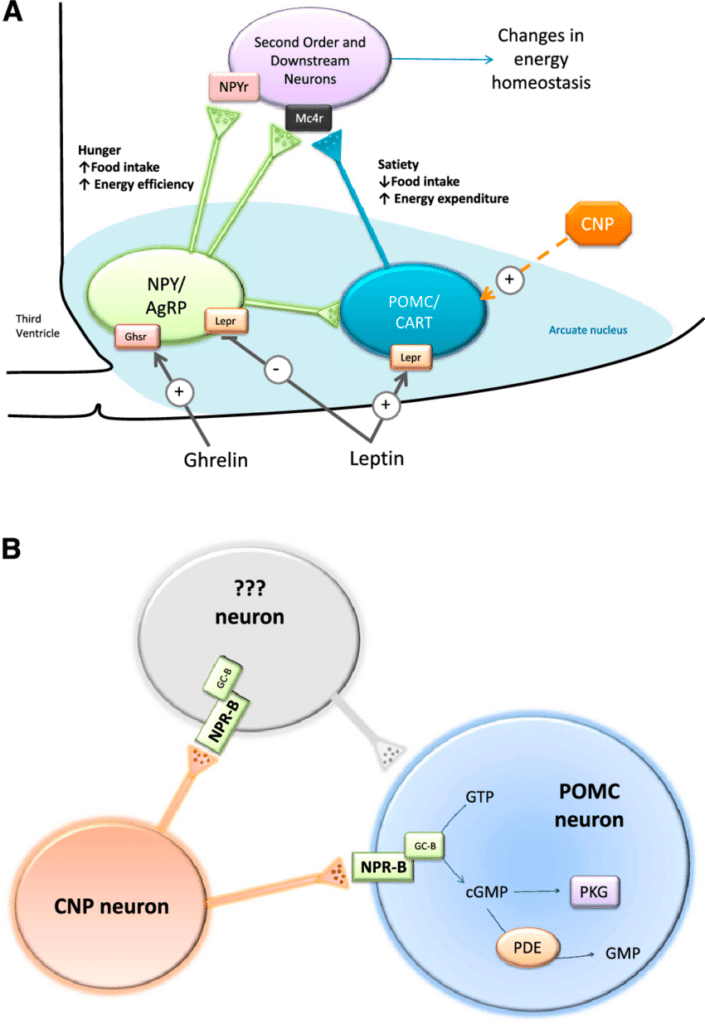
Leptin may also act in conjunction with other satiety signals such as CCK and GLP-1 at a different area of the brain to further promote satiety.
Leptin also interacts with the hedonic eating system, and not just the homeostatic eating system. The hedonic eating system deals more with cravings and desire to eat and not just physiological hunger. We know that dopamine has a significant role in the hedonic drive to feed. Leptin also interacts with the dopamine system to reduce the hedonic drive to feed, so leptin has effects in decreasing physiological hunger pangs but also probably has effects in decreasing cravings as well.
In studies of completely leptin deficient mice, and also in observations of humans with congenital leptin deficiency, we always see the same thing: Extreme drive to eat combined with obesity as well as a low energy expenditure. Individuals that are leptin deficient respond well to leptin treatment, however individuals that are already obese with high levels of leptin do not respond to this, indicating leptin resistance.
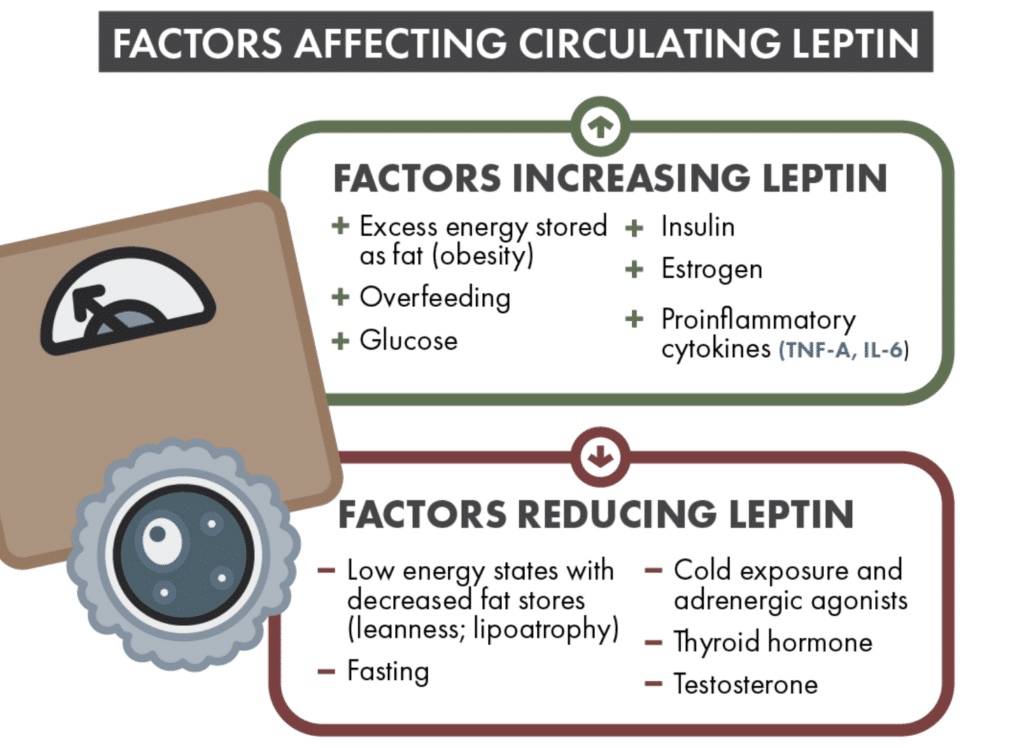
Leptin’s Response to Increasing or Decreasing Calories
In an extended fast (as little as 3 days), leptin levels drop significantly (some range in studies appears to be from 60-500%) regardless of bodyfat level. This may be a tactic of leptin resistance reversal in the obese, but we’ll talk about that a little more later.
Leptin levels also decrease in caloric restriction combined with exercise, but not to as much of an extent, indicating that leptin is not only regulated by body fat stores but also acute energy status.
A more moderate calorie deficit will lead to preservation of leptin levels for much longer than a steep calorie deficit, so this is also an argument for a longer, slower diet instead of a super steep deficit right off the bat for an individual without leptin resistance.
Increasing Leptin Levels Restores Thyroid and Sex Hormones in Starved Individuals
We know leptin levels become very low when someone is extremely lean and that metabolic adaptation occurs when one is extremely lean, but this also happens in extended fasting regardless of body fat levels.
In the example of a 3 day fast we talked about earlier, as leptin falls, we see a decrease in sex hormones, increase in cortisol, decrease in thyroid hormone, and decrease in IGF-1 levels. However, physiological doses of leptin administered as a drug to people in this state restores proper levels of these hormones.
For a little more data, Leptin administration restores thyroid hormone, testosterone and luteinizing hormone (LH) levels in fasted mice, and LH pulsatility and testosterone levels in starved human volunteers.
For how it works mechanistically, for sex hormones: Leptin increases GnRH (gonadotropin releasing hormone → The first upstream hormone responsible for production of testosterone, estradiol, progesterone, etc) through indirect actions at the hypothalamus.
For thyroid hormone, leptin acts to increase TRH (the first domino in creation of thyroid hormone) in the hypothalamus. In women with hypothalamic amenorrhea, leptin administration increases free T3 and T4 levels but not TSH levels (a good thing). Leptin administration to weight-reduced individuals reverses the declines in T3 and T4 levels and in energy expenditure that are seen after a dieting period.
At this point, you may be wondering why leptin isn’t a drug of abuse in bodybuilding competitions or those dieting hard in order to preserve thyroid and testosterone function. It just so happens to be one of the top 3 most expensive drugs in the world, so this is more than likely the reason.
Leptin’s Regulation of Metabolism
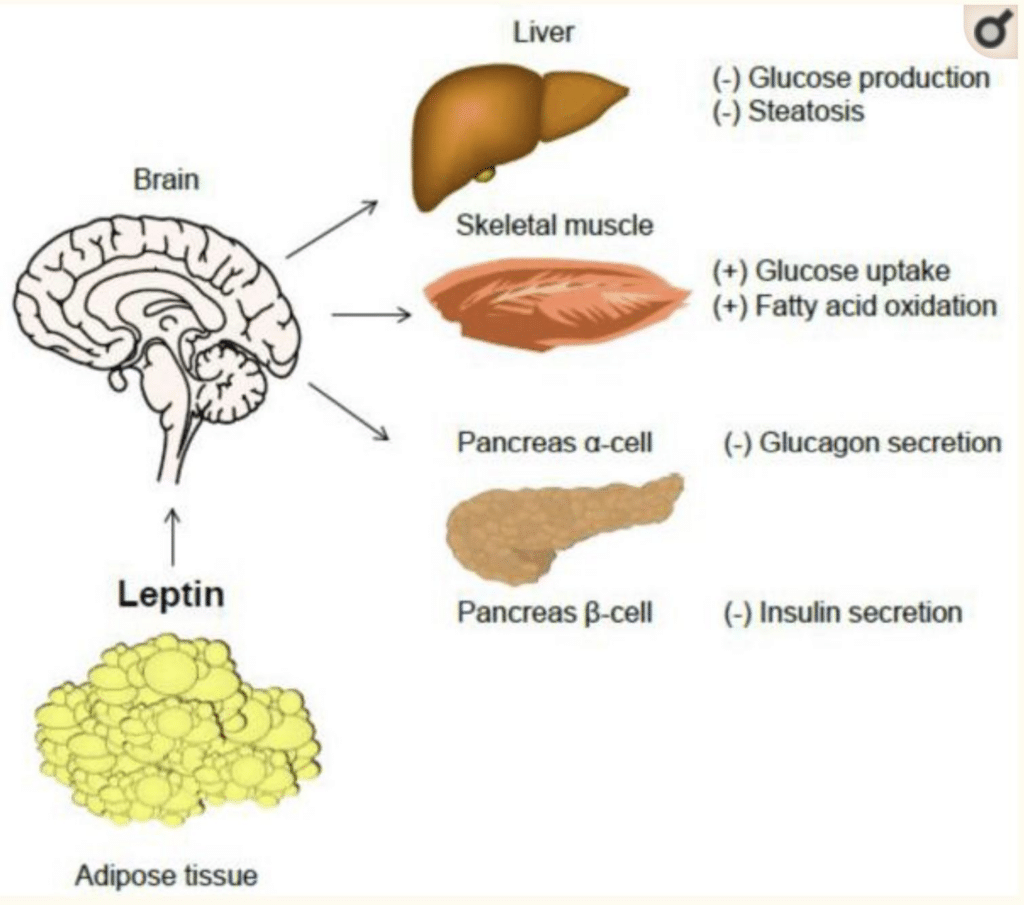
Glucose metabolism
Leptin can have a normalizing effect on blood sugar by both decreasing hepatic gluconeogenesis (creation of blood sugar from proteins) in states of overproduction of glucose (like metabolic syndrome/type 2 diabetes) and also by increasing insulin sensitivity.
Leptin also interplays with insulin in that it has an effect of decreasing both the production and secretion of insulin, normalizing insulin release to current body fat levels. Insulin also stimulates leptin production and secretion.
Fat or lipid metabolism
Leptin administration has been shown to decrease de novo lipogenesis (creation of fat in the liver from other substrates such as carbohydrate) and stimulates lipolysis and subsequent fatty acid oxidation, which translates to more fat burning.
Bone Metabolism
Leptin also has a role in bone mineral density through its effects on IGF-1 and possibly others. For example, leptin treatment increases markers of bone formation, bone mineral density and content in the lumbar spine of patients with hypothalamic amenorrhea.
Immune function
Various studies have shown that leptin has important roles in modulating innate and adaptive immunity. Leptin stimulates neutrophil chemotaxis and promotes macrophage phagocytosis, as well as appropriate production of pro-inflammatory cytokines such as interleukin (IL)-6, IL-12, tumor necrosis factor (TNF)-α.
Production of inflammatory cytokines doesn’t sound great, but this is appropriate production, meaning that the inflammatory cytokines are produced in the face of things they’re needed for, like fighting infections.
Recently, it has also been shown that leptin acts as a negative signal for the proliferation of regulatory T cells, while stimulating T helper 1 cell, which translates to less autoimmunity.
Thus, leptin may contribute to the protection from infections and the development of autoimmunity.
Exercise
Leptin receptors and leptin signaling in skeletal muscle, particularly in the leg muscles, are reduced in obese subjects, suggesting a potential mechanism of peripheral leptin resistance in obesity.
Sprint exercise or intense intermittent exercise activates AMPK, which is also activated by leptin in human skeletal muscle. Moreover, sprint exercise under fasting conditions enhances leptin signaling in human skeletal muscle. Given its high intensity nature, it could be extrapolated that resistance exercise may have the same effect.
This has implications for helping reverse some aspects of leptin resistance in the obese individual.
Conversely, in healthy volunteers, one week of bed rest resulted in an increase in circulating leptin level without a concomitant increase in markers of leptin signaling in leg skeletal muscle, indicating an induction of leptin resistance in skeletal muscle with inactivity.
Moral of the story here is that any sort of activity is going to help normalize leptin signaling, particularly in obese individuals with leptin resistance, from low grade walking up to sprint exercise and resistance training.
States of Disrupted Leptin Signaling and Applications
Here are some of the most common areas where you might see altered leptin signaling in clients:
Leptin in the Super Lean Individual (or Chronically Under-eating/Overtraining)
Low leptin levels are part of the metabolic adaptation seen in the super lean or those that have been excessively dieting for long periods of time. If we look at some of the factors that increase leptin: overfeeding, glucose, and insulin, we can see why things such as single or multi-day refeeds have been slightly efficacious in mitigating metabolic adaptation to some degree.
Taking diet breaks (several weeks at maintenance) might be able to help as well. However, while these tactics transiently elevate leptin levels and mitigate this to a small degree, truly restoring normal leptin levels and thus normal endocrine function and energy homeostasis would take increasing calories for longer periods and gaining a little of that bodyweight back (aka a reverse diet).
When someone is in the process of dieting, this is a case for a more mild deficit; fasting regardless of adipose status drops leptin levels a very large amount, very fast (60-500% within a 3 day fast). Although caloric restriction does this as well, studies also show that both the degree of leptin dropping and time it begins to drop depends on the severity of the caloric deficit.
There are also studies showing the steeper the deficit, the more the lean mass is lost, which lines up with the other hormones we know that leptin effects (testosterone, IGF-1). Therefore, it seems that the slower you can diet, the better it will be for feelings of well-being, libido, sleep, retention of lean mass, and preservation of current energy expenditure. Keep in mind you can still diet a bit faster for obese individuals.
This can be especially true for women who want to retain their cycle during a dieting or training phase. Remember, when leptin treatment was used in extremely lean women with loss of cycle, it restored levels of not only their sex hormones, but also thyroid hormones and energy expenditure.
Yes, when extremely low levels of bodyfat are achieved because of a physique show or any other reason, it is extremely likely that a woman will lose her cycle regardless of the speed of dieting, but there are also cases of women losing their cycle from extreme diets when they haven’t reached these low bodyfats yet.
This could be due to the drops in leptin observed by an extreme calorie deficit. For the average dieter just looking to get decently lean, a more moderate deficit will certainly preserve cycle health the entire way down.
For the physique competitor, it will certainly preserve cycle health and hormonal levels as far down as possible. In any case, if a woman has hypothalamic amenorrhea for a reason other than dieting, leptin treatment may be an option to seek in order to restore levels of sex hormones.
Leptin Dysfunction in the Obese Individual
Just like obese individuals experience insulin resistance, they experience leptin resistance at the level of the brain and these effects mimic states of very low leptin given the brain cannot see the signal. They also experience peripheral muscular leptin resistance.
Interestingly, many studies detail the same leptin-lowering effect from dieting in obese individuals, however it comes without a decrease in resting metabolic rate.
That’s because this profile of individual already likely has lower than expected resting metabolic rates and energy expenditure due to leptin resistance. If we look at the mechanisms causing leptin resistance: inflammation and endoplasmic reticulum stress, we can start to do or look at things that may help reverse this.
It bears emphasis that all of the following considerations should happen in conjunction with a weight loss plan. Doing some of the following without fat loss may help slightly, but these should be thought of in the context of concurrent weight loss and bodyfat reduction (hypocaloric diet).
Ensuring that the individual has a good micronutrient status all the way around will help decrease inflammation in many different ways; from decreasing oxidative stress from adequate vitamin C, vitamin E, B vitamins, selenium, manganese, copper, and iron, to cardiovascular health by magnesium/K/D and others, to regulation of proper immune function by vitamin D, zinc, and many of the aforementioned vitamins as well. That’s by no means comprehensive, there’s many other ways optimizing micronutrient status can help with this.
Next, we can look at blood sugar control: consistent blood sugar and insulin spikes as well as high basal levels of those things over time cause significant inflammation. Therefore, anything we can do for blood sugar control would help: Setting an appropriate carbohydrate level for activity and increasing protein intake and fiber intake at meals with starchy carbohydrates to slow digestion.
Supplements that may help with blood sugar control and therefore inflammation associated with it would be berberine HCl, ceylon cinnamon, bitter melon extract, or chromium. This could be a case for a ketogenic diet as a temporary tool (but not permanent lifestyle) if the individual finds it easy to adhere to: we know a keto diet drastically reduces inflammation in those with metabolic syndrome and can be a faster way to expedite the process.
Instituting a time restricted feeding protocol can help here as well, particularly an early time restricted feeding protocol. Cutting off food 3-5 hours before bed has been shown to improve metabolic health even if weight loss isn’t achieved, and that includes leptin.
Very high triglycerides have been shown to hamper leptins actions, so besides weight loss, we know marine omega 3’s have the most potent effect on reduction of triglycerides, so may help with this while weight loss is occurring. Curcumin also may have a mild effect on triglycerides and also an effect on systemic inflammation.
For the aspect of endoplasmic reticulum stress, there is some data in mice showing that the supplement TUDCA helped reverse leptin resistance via reduction in endoplasmic reticulum stress, although this has not been tested in humans.
Since TUDCA has many other beneficial effects throughout the body, especially the liver (which many people with metabolic syndrome also have some degree of NAFLD as well) if someone has the expendable income, it may be worthwhile to try out at 1000mg/day.
Gut issues are also a consideration. We also know those with gut issues such as IBS, SIBO, etc have increased systemic inflammation from this, so addressing gut issues in conjunction with weight loss can help reduce systemic inflammation and aid in both weight loss and leptin resistance reversal.
Visceral fat is also a target here. Visceral fat is a huge contributor to both metabolic syndrome and leptin resistance. Visceral fat is inflammatory in nature and has been shown to put out much higher levels of leptin than subcutaneous adipose tissue.
Weight loss itself will reduce visceral fat, however exercise preferentially causes visceral fat loss first over subcutaneous, so including exercise in a weight loss regimen can significantly help with this. Another plus for a ketogenic diet for a time period: many studies have shown significantly more visceral fat loss earlier on in the diet on a ketogenic diet for obese individuals than mixed diets. Again, it bears repeating this would be useful for a time period, not a permanent lifestyle.
Sleep and circadian hygiene will also play a huge part in reversing leptin resistance. It might be a little more common knowledge that sleep restriction, regardless of bodyfat level or energy intake, decreases leptin levels. Optimizing sleep at any point in time, but especially during a weight loss phase, is very important.
However, recent research in mice (I couldn’t find any in humans yet) suggests that chronic jet lag situations, which we would also see in night shift work, can clearly induce leptin resistance regardless of sleep hours. Although this has not been shown in humans yet, when someone is sleeping less and also in situations of chronic jet lag or shift work, we may have a seriously deleterious combination of lower circulating levels along with leptin resistance regardless of BMI.
Finally, psychological and emotional stress tops it all off. We know stress in general can contribute to chronic, low-grade inflammation, so addressing psychological and other stressors may help with leptin resistance.
In summary, there is a case for a low carb or possibly ketogenic diet if the person can adhere easily given its preferential decrease in visceral fat and innate ease of blood sugar control. This isn’t necessary though, and is of course pending activity levels.
Ensuring good micronutrient status is also important (this should be especially paid attention to if doing a ketogenic diet given its restrictions).
Exercise as part of a weight loss regimen will speed up leptin resistance reversal.
Otherwise controlling blood sugar by moderating carbohydrate intake and increasing protein and fiber at meals. Addressing gut issues should be done, as well as any sort of lifestyle stresses.
Supplements that may help on the way down include any micronutrients that have gaps in the diet (should probably supplement D + K2 given their absence in diet), EPA/DHA from fish oil, blood sugar control supplements such as berberine HCl, bitter melon extract, chromium, or ceylon cinnamon. Curcumin and TUDCA may have an application here as well.
Conclusion
As you can clearly see, leptin is an unsung hero of hormones within the body; a hormone pulling the strings of our thyroid hormone, sex hormone axis, and potentially even HPA axis behind the scenes. In general, low levels of bodyfat and current very low energy status (fasting or a super steep deficit) regardless of bodyfat levels will lower leptin.
On the other hand, obese individuals experience very high levels of leptin and resistance to the hormone. In the former situation of very low bodyfat, a reverse diet is necessary to get folks up to normal leptin levels, whereas all of the lifestyle aspects I mentioned for the obese individual may be able to help reverse leptin resistance.