Introduction – The Importance of Gut Health
If you have a client that’s struggling to reach a fitness goal; whether that be hitting a PR in the gym or getting to that level of leanness they’ve always wanted (or both!), troubleshooting gut health can be a major missing piece of the equation.
Keeping the gut in a healthy state has far-reaching implications across the entire body. Connections to other organ systems include the gut-brain connection, gut-thyroid, gut-metabolism, gut-sleep, and more.
Meaning, if your gut is in a bad place, this can be contributory to brain fog, depression, anxiety, weight loss plateaus, poor exercise recovery and having a tough time putting on muscle, insomnia, and contributes to numerous chronic diseases.
Although this post is mainly about the benefits and use cases of pre-, pro-, and postbiotics, the first thing I would encourage coaches and the general population alike to do is get out of a quick fix mindset here. If we go towards a probiotic, yet we’re still sleeping 5 hours a night, eating hyper processed foods on a daily basis, and not exercising, we’re putting a bandaid on an amputation here.
That being said, if someone is in a physiological hole in terms of gut health and are seemingly doing everything right, meaning eating mostly whole foods with a good amount of fiber, exercising, sleeping well, and managing stress, then there are certainly use cases for these supplements in the context of an overall lifestyle protocol.
We do have a 4 part series on gut health, including what good digestion actually is, stomach acid and bile, dysbiosis, and leaky gut, so please check that out as well.
What are They?
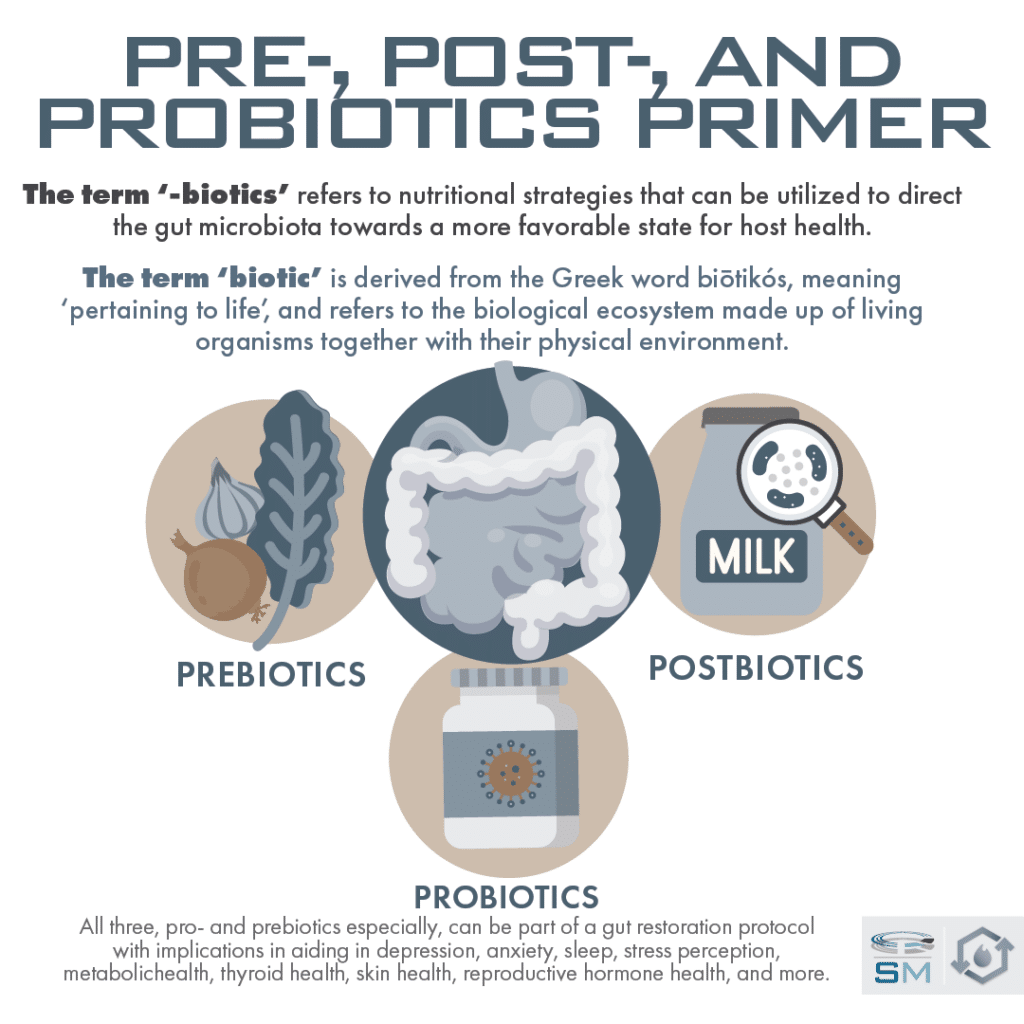
Probiotics are a live-organism class of supplement that can confer a health benefit to the host and have been shown to aid in conditions such as IBS and SIBO.
Prebiotics are substrates that are directly utilized by the body’s microorganisms to foster a healthy microbiota and confer benefit to the host.
Postbiotics are a newcomer to the game; these are the products of bacterial fermentation in the gut such as short-chain fatty acids, microbial fractions, functional proteins, cell lysates, extracellular polysaccharides, and more. Basically, its bacteria poop. These may increase their potency when administered with live microorganisms or probiotics.
All three, pro- and prebiotics especially, can be part of a gut restoration protocol with implications in aiding in depression, anxiety, sleep, stress perception, metabolic health, thyroid health, skin health, reproductive hormone health, and more.
Probiotics
If you mention probiotics to a random individual, you’ll probably get a wide range of emotional responses. Some will say they totally saved their gut health, some will say they did absolutely nothing for them, whereas others will say they made their symptoms significantly worse.
These are all valid experiences and things that can happen. There are tons of variables and complexity to consider: The individuality of someone’s microbiome and gut issues, the types and strains of the probiotic, the brand quality of the probiotic (some may not even have whats on the label or may be contaminated), and other considerations.
This is why choosing when and how to use a probiotic, as well as what class, can be confusing. This post is designed to educate you on the different classes and use cases, as well as what to do with any potential negative reactions.
Probiotics aren’t relegated to capsules; any fermented food will contain usually 5-10 different strains of probiotics. These foods include yogurts, kefir, natto, some fermented cheeses, and kombucha. If you’re relying on something like sauerkraut or pickles for your probiotics, you have to make sure to get truly fermented and unpasteurized products, which is rare.
Let’s go ahead and drill into probiotic supplements. What most people do not realize and what’s not marketed is the fact that there are three broad classes of probiotics, with hundreds of probiotics within each class, with potential different use cases for each, so let’s delineate between.
Probiotics: Classes and Functions
One particular misconception about probiotics that people have is that they’re actually colonizing us and directly replacing gut bacteria that we’ve lost. Most probiotics do not actually colonize the gut, and health benefits do not hinge on colonization.
For instance, purposefully heat-killed probiotics (referred to as Tyndallized probiotics in scientific literature) still conferred many benefits to the host in several different human RCTs including for treatment of diarrhea, IBS, atopic dermatitis, and more.
How do they work if they’re not actually colonizing? The Journal of Clinical Gastroenterology gives these points:
- Increase microbiota diversity and phylotypes as they pass through
- Decrease pathogens and their toxins as they pass through
- Alter bacterial community structure to enhance evenness and promote more rapid recovery from imbalance
- Directly inhibit harmful microbes through a variety of mechanisms like the production of antibacterial compounds and also by promoting immune responses against specific microbes.
- Promotes a healthier gut environment for a healthier microbiota: stimulating intestinal mucus production, enhancing gut-barrier effects, and reducing gut inflammation.
- Perform enzymatic metabolism of host compounds such as bile salts and ingested xenobiotics (toxins)
- Increase antioxidant status and micronutrient status of the host. Probiotics can contribute to a microbiome that creates more vitamins K2, thiamin, riboflavin, pantothenic acid, biotin, and folate.
Additional mechanisms of action:
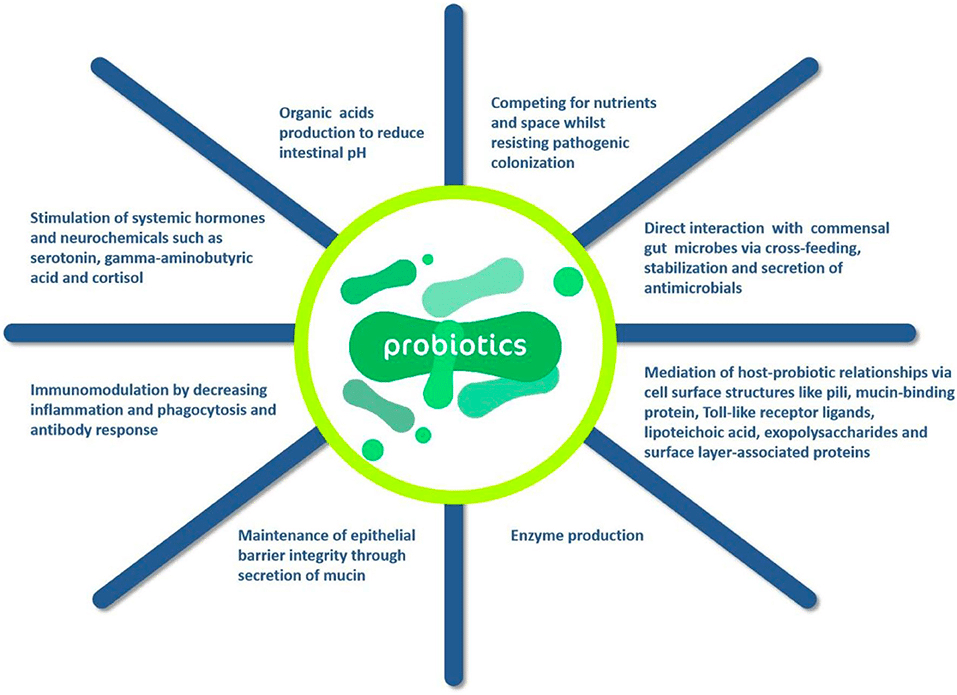
Source: Siyong You et al 2022
Lactic Acid Producers (Lacto/Bifido blends)
These are more easily identifiable than you might think; just take a look at the back of the ingredient label and if most of the strains start with lactobacillus and bifidobacterium, then its a lacto/bifido blend. These are the most common probiotic products.
Lactic acid producers have the largest body of evidence behind them and are generally one of the first lines of defense alongside lifestyle intervention for cases of IBS, SIBO, etc. We will go over the data in a subsequent section.
Most lactobacilli are transient and do not colonize, but are important. Lactobacillus acidophilus (seen in many probiotics) is not a regular resident of the gut, but appears to provide benefits. Many other lactobacilli species are permanent residents, however.
Lactobacilli either produce one thing (lactic acid) from fermentation, or different things (lactic acid, other gases such as CO2). Why is this relevant? People with negative overgrowths, such as SIBO, may have an overgrowth of heterofermentative which causes excess gas production and bloating.
Bifidobacterium are residents of the large intestine; there’s about 30 different bifidobacterium species that we’ve currently identified there. It is widely accepted that they are established through breastfeeding. Bifido strains provide numerous health benefits from intestinal barrier function to protection against colon cancer.
Other strains that may be included in lacto/bifido blends as lactic acid producers are E. Coli, Streptococcus (thermophilus), Enterococcus, and Pediococcus strains.
Soil-based or Spore forming
These are monikered from the fact they spend most of their life cycle dormant as a spore in soil. The hypothesis is that they replace what we may be missing from reduced contact to dirt/soil in our modern lifestyles.
If you look at the back of your probiotic and see that most strains start with “bacillus”, then you’ve got a spore-forming probiotic. Common strains in spore-forming probiotics are normally bacillus subtilis and bacillus coagulans.
There is a bit less of a body of evidence behind spore-forming probiotics, but they’ve also been shown to help rebalance and improve host microbiota and may be best used alongside a lacto/bifido blend.
Fungal-Based
By far the most common species within this class is Saccharomyces Boulardii. S. Boulardii is not part of the normal gut microbiota, and does not colonize the host. It is not affected by stomach acid or bile, but is actually a lactic acid producer as well.
Has been shown to successfully treat diarrhea, aid in C diff treatment, prevent relapse of Crohn’s, and as an adjunct treatment for IBD.
One particularly useful function of S. Boulardii is that it has antifungal effects and can disrupt fungal biofilms, meaning this is one of the primary intervention’s we’d use in cases of candida overgrowth.
S. Boulardii has also shown effectiveness for certain parasites such as Blastocystis Hominis and giardia as well, whether alone or with antibiotics. In many cases, individuals have to take a course of prescription antibiotics for these parasites, but literature actually shows better eradication of these infections when antibiotics are administered with S. Boulardii rather than just antibiotics alone.
Now let’s dive into a quick summary of evidence, followed by a translation to application of how we’d actually use these things.
Summary of Evidence with Probiotics:
Summary of Evidence with Probiotics:
- IBS: A couple meta-analyses showed good efficacy for treatment of IBS with little to no side effects. Most studies are from a lacto/bifido blend, with better results seen with the inclusion of bifidobacterium infantis.
- An updated 2023 meta-analysis has worked out optimal doses of each class for IBS:
- The optimal dose of a lacto/bifido blend specifically appears to be 10 billion CFU.
- Saccharomyces boullardi’s optimal dose seems to be between 10-15 billion
- Soil-based falls between 2 – 6 billion.
- An updated 2023 meta-analysis has worked out optimal doses of each class for IBS:
- SIBO: Meta analyses show both lacto/bifido blends and soil-based to be effective in treatment of SIBO; lacto/bifido alone was better than soil-based alone, but there may be a greater effect when both are used. Similar dosages to the above were used.
- A recent 2019 study tested probiotics effect on symptom remission in those with IBS WITH confirmed SIBO vs. those with IBS confirmed WITHOUT SIBO. The individuals with SIBO experienced a 73% improvement in symptoms, whereas those without SIBO experienced an 11% improvement in symptoms.
- This tells us probiotics may be especially efficacious in instances of SIBO, which is counter to a common thought in the functional health space that we shouldn’t use probiotics in cases of SIBO.
- IBD: Lacto/bifido, S. Boullardi, and E. Coli Nissle 1917 showed good effects for treatment with IBD. Best approach for a natural approach was seen with these strains plus herbal antimicrobials.
- Weight loss: Minimal but noticeable. Best results saw 2.2-3.7lb loss over a several weeks time. Strains were lactobacillus gasseri at 100 billion CFUs and lactobacillus rhamnosus at 320 million CFUs.
- Diabetes – Reductions in blood sugar ranging from 5 to 16 points was the average effect of a combination of probiotics in studies – prebiotics appear better at treatment of diabetes than pro.
- Mood/fatigue – Meta analyses showed positive effects on stress hormone levels, depression, anxiety, fatigue, and hostility, mostly with lacto/bifido blends
Translation and Application
Probiotics can be a helpful addition to a treatment protocol for numerous conditions, gut or otherwise. However, with gut conditions, it is always best to find the right type of diet to reduce or eliminate whatever damage the diet is causing, whether it be barrier-related or bacterial overgrowth related. In many cases with the gut, just putting a probiotic on top of a western american diet or a diet that is causing damage will not cause relief.
Lacto/bifido blends are the most studied and may provide great relief for the above conditions. Saccharomyces is best used for diarrhea, candida, and may also help IBS/SIBO.
Soil based has also shown good results with SIBO/IBS, especially in conjunction with lacto/bifido blends. Doing a “triple therapy” with all 3 has been used in some studies with good results and little side effects. May not be necessary, but if the client has the budget, it may be worth trying all 3 classes at once.
Important note: Negative reactions to probiotics can happen. Sometimes these are just die-off, or Herxheimer reactions, but sometimes that particular probiotic just doesn’t jive with the individuals internal health at the time.
Herx reactions generally last anywhere from 3 days to 2 weeks, but in the vast majority of cases, they dissipate in around 4-5 days. The practitioner rule of thumb that I’ve seen is that if symptoms don’t get better within 2 weeks max, then it is most likely a negative reaction and not a Herx reaction, and to remove the probiotic and try a different class.
Prebiotics
Prebiotics are broadly defined as a non-digestible substrate that stimulates the growth or activity of beneficial bacteria in the large intestine. Basically, these are the fibers or substances that feed your gut bugs. There are some caveats around supplementing prebiotics though, which we’ll get to down below.
The most widely accepted prebiotics are fermentable oligosaccharide inulin, fructooligosaccharides (FOS or fructans), galactooligosaccharides (GOS), or lactulose. There are many other types of candidate prebiotics such as resistant starches (created in the process of cooking and cooling/refrigerating starches like rice, pasta, etc), acacia fiber, xylooligosaccharides, glucooligosaccharides, and many more.
Caution: There’s been a big prebiotic craze lately on the premise that feeding your gut bacteria is always beneficial. However, in the case of SIBO and in many cases, generalized IBS as well, prebiotics might have to be avoided until overgrowths have been trimmed down as they can feed negative bacterial overgrowths as well. Low prebiotic diets like the low FODMAP or SCD are now part of the standard of treatment for SIBO/IBS.
Examples of high prebiotic containing foods are garlic, onions, dandelion greens, chicory root, jerusalem artichokes, green bananas and green plantains, whole oats, many cooked and cooled starches (creates resistant starch) such as rice, and apples (skin). If you notice your gut symptoms get significantly worse after eating these, you may need to follow a low FODMAPs diet for a while as part of an intervention to get your gut back to a healthy place.
In cases where they’re not contraindicated, studies show better health of gut mucus membranes, lowered cholesterol, insulin, blood sugar, and inflammation with prebiotic supplementation.
In individuals without SIBO, prebiotics show great promise in metabolic syndrome and diabetes situations with the improvements described above. Prebiotics can be a good part of a gut healing protocol later on in the protocol after overgrowths have been trimmed and appropriate bacterial balance has been achieved in order to feed the beneficial bacteria.
Postbiotics
Newcomers to the supplemental game in any case, postbiotics are defined as the metabolites formed upon bacterial fermentation within the gut. In other words, its basically what bacteria poops out after it’s finished digesting your fiber and other prebiotics.
These include but not aren’t limited to: short-chain fatty acids (SCFAs), microbial cell fractions, functional proteins, extracellular polysaccharides (EPS), cell lysates, teichoic acid, peptidoglycan-derived muropeptides and pili-type structures
Postbiotic Mechanisms
Mechanisms by which these provide benefits have not been fully hashed out, but we do have a little bit of preliminary data.
In terms of immune function, fermented postbiotic products from strains Bifidobacterium breve C50 and Streptococcus thermophilus 065 have demonstrated longer survival of positive immune cells, lower levels of pro-inflammatory cytokines, and higher levels of anti-inflammatory cytokines, suggesting anti-inflammatory immune system stimulation.
Cytokines are like the hormones of the immune system; pro-inflammatory ones send a message to immune cells “Hey, come over here and create inflammation!” and anti-inflammatory ones do the opposite.
Postbiotics from the same strains I just discussed have been shown to improve the epithelial barrier function and stimulates positive branches of the immune system in mouse models highlighting the involvement of postbiotic components in host immune function.
Two other fermentation products associated with health benefits are exopolysaccharides (EPS) and extracellular vesicles (EVs). In vitro and animal studies (no human data yet) of these particular fermentation products suggest cardioprotective, anti-ulcer, anti-tumor, antioxidant and cholesterol lowering effects but clinical trials need to be performed.
Postbiotics are Most Studied in the Elderly and Infants
The main populations of humans that have been studied with postbiotics are infants and the elderly. Fermented infant formulas (FIFs) have been studied fairly extensively. These are usually made by fermentation of follow-on infant formulas by lactobacillus genera. There is a large need here, since breast milk contains a huge amount of both probiotics and postbiotics, and is partially responsible for cementing the infants microbiome.
As far as beneficial effects, FIFs have been shown to have a positive effect on infant immune development and function over regular formula and positive effects for recovery of diarrhea episodes as well as less frequency of them.
Studies with postbiotics in elderly humans are also positive, ranging from positive effects on immune function, barrier functions, improvement in stool consistency as measured by bristol stool chart, and improvements in mucus membrane.
Remember how I mentioned earlier that heat-killed probiotics still showed beneficial effects? It may be that the postbiotics are what’s conferring benefit when heat-killed probiotics are administered (still lots of debate).
The bottom line with postbiotics is that it is a very new body of literature; the term doesn’t even have a clear definition yet, or range of what it encompasses. We know and have identified certain postbiotics, but research is still very new.
The vast majority of research is in vitro and in animal studies, however studies with babies using FIFs and in elderly using different fermented drink products are promising in regards to multiple things, but mainly immune function.
As far as supplementation with postbiotics, since these are so new and with limited research, any product claiming to contain postbiotics should be regarded with caution. I would personally wait till more RCTs are done with certain metabolites before jumping into supplementation.
Conclusion
Once again, as we close out, I want to emphasize the fact that if someone is suffering from distressing gut issues, diet and lifestyle change is going to make 80-90% of the difference. Supplemental probiotics are probably the most efficacious and studied in terms of being an adjunct to lifestyle for remediation of gut issues. In most cases, we start with a quality lacto/bifido blend, unless we know there is presence of candida or its fairly severe IBS-D, then we might want to go the route of S. Boulardii. Triple therapy with all three classes is an option.
Prebiotics will be highly dependent on use case and whether or not they make gut issues worse. If you know you react to the foods I mentioned in the prebiotics section, I would avoid prebiotics until the overgrowth is taken care of. Otherwise, they can be a good adjunct to a fruit and vegetable-rich diet to maintain a healthy microbiome.
Postbiotics are more of a grey area. Not only do we not have much research; the research scientists are using tested and proven postbiotics to conduct their studies. The consumer supplement market, on the other hand, is well known for contamination of products, not having the doses listed on the label, and more issues. Until we have both good research and proven brands and products, I would avoid these.
References
- Carrie Wegh et al. “Postbiotics and Their Potential Applications in Early Life Nutrition and Beyond.” PMID: 31547172
- Jelena Vulevic et al. “A mixture of trans-galactooligosaccharides reduces markers of metabolic syndrome and modulates the fecal microbiota and immune function of overweight adults.” PMID: 23303873
- Leventogiannis, K., Gkolfakis, P., Spithakis, G. et al. Effect of a Preparation of Four Probiotics on Symptoms of Patients with Irritable Bowel Syndrome: Association with Intestinal Bacterial Overgrowth. Probiotics & Antimicro. Prot. 11, 627–634 (2019). https://doi.org/10.1007/s12602-018-9401-3
- Parvin Dehghan et al. “Oligofructose-enriched inulin improves some inflammatory markers and metabolic endotoxemia in women with type 2 diabetes mellitus: a randomized controlled clinical trial.” PMID: 24332524
- Nicole Kellow et al. “Metabolic benefits of dietary prebiotics in human subjects: a systematic review of randomised controlled trials.” PMID: 24230488
- Sailendra Nichenametla et al. “Resistant starch type 4-enriched diet lowered blood cholesterols and improved body composition in a double blind controlled cross-over intervention.” PMID: 24478107
- Edna Nyangale et al. “Bacillus coagulans GBI-30, 6086 Modulates Faecalibacterium prausnitzii in Older Men and Women.” PMID: 25948780
- Shira Doron and David Snydman “Risk and Safety of Probiotics.” PMID: 25922398
- EB Avalueva “[Use of Saccharomyces boulardii in treating patients inflammatory bowel diseases (clinical trial)]” PMID: 21033091
- Charlotte Hedin et al. “Evidence for the use of probiotics and prebiotics in inflammatory bowel disease: a review of clinical trials.” PMID: 17637082
- Anna Krasowska et al. “The antagonistic effect of Saccharomyces boulardii on Candida albicans filamentation, adhesion and biofilm formation.” PMID: 19732158
- Bulent Besirbellioglu “Saccharomyces boulardii and infection due to Giardia lamblia.” PMID: 16798698
- Mary Ellen Sanders “Impact of probiotics on colonizing microbiota of the gut.” PMID: 21992949
- R Spiller “Review article: probiotics and prebiotics in irritable bowel syndrome.” PMID: 18532993