Menopause marks the end of reproductive years once your ovarian follicles become less viable and the number of eggs you have nears zero. This results in low levels of various hormones, including estrogen and progesterone.
On average, in the US, menopause starts around age 51, and the hormonal changes that result predispose women to osteoporosis, increased risk of heart disease and stroke. Hypothyroidism and metabolic syndrome are greater post-menopause as well.
The lack of female sex hormones also causes body fat redistribution – less storage around the hips and thighs and more around the belly. It also makes it a bit harder to hit fat loss and muscle gain goals, and some women gain weight.
There are, however, things we can do to combat this and help our clients have a healthy menopause experience.
Table of Contents
Why Does Healthy Menopause Matter to Fitness Coaches?
Women who have gone through menopause will tend to have a harder time getting results than premenopausal women. They also deal with the symptoms of having a lower sex hormone status.
Menopause symptoms include hot flashes, night sweats, palpitations, headaches, insomnia, fatigue, bone loss, low libido, vaginal dryness, depression, anxiety, mood shifts, lack of motivation, and difficulty with memory recall.
These changes affect quality of life, which may, in turn, affect adherence and makes body composition changes slightly harder. It’s important to understand the changes that occur with menopause so that you can better tailor a plan to your postmenopausal client.
Hormone Replacement Therapy
Many of these changes can be reduced through a hormone replacement therapy (HRT) regimen postmenopause. It’s even advised by many practitioners to begin hormone replacement when one is solidly in the menopausal transition and is experiencing symptoms of erratic hormone levels.
Those reading might have concerns about reported risks involved with hormone replacement therapy, such as breast cancer or stroke. All of these concerns came from the large Women’s Health Initiative study in the early 2000s, who’s execution and interpretation was one of the larger blunders of medical science in the past 50 years.
This article isn’t necessarily about the in’s and out’s of women’s HRT; we have a separate article that dives into that quite in-depth, so if you’d like to check that out and learn why the WHI study was less than reliable, and learn more about the optimal HRT regimen, check it out here.
In a nutshell, however, bioidentical, transdermal (cream or patch) estradiol and bioidentical, oral micronized progesterone is the optimal HRT route and delivery system, and the earlier you start it (within 10 years of entering menopause), the better off you will be from a health perspective.
Menopause Symptoms
Women typically begin the menopause transition or notice progression towards menopause at some point in their 40s but can experience symptoms early as their late 30s. Anything above 42 is considered normal, and before that is “early perimenopause,” which happens to about 1 in 100 women.
Here are a few signs of perimenopause:
- Irregular cycle length and missed cycles become more common; early in the transition, many women experience shorter cycles (<25 days), however, cycles may be longer later in the transition.
- FSH levels become elevated because the brain is trying to stimulate the ovaries to mature a follicle, but the ovaries are not responding as well anymore.
- LH levels also rise, attempting to stimulate the ovaries to produce enough estrogen, but tend to lag behind FSH elevations.
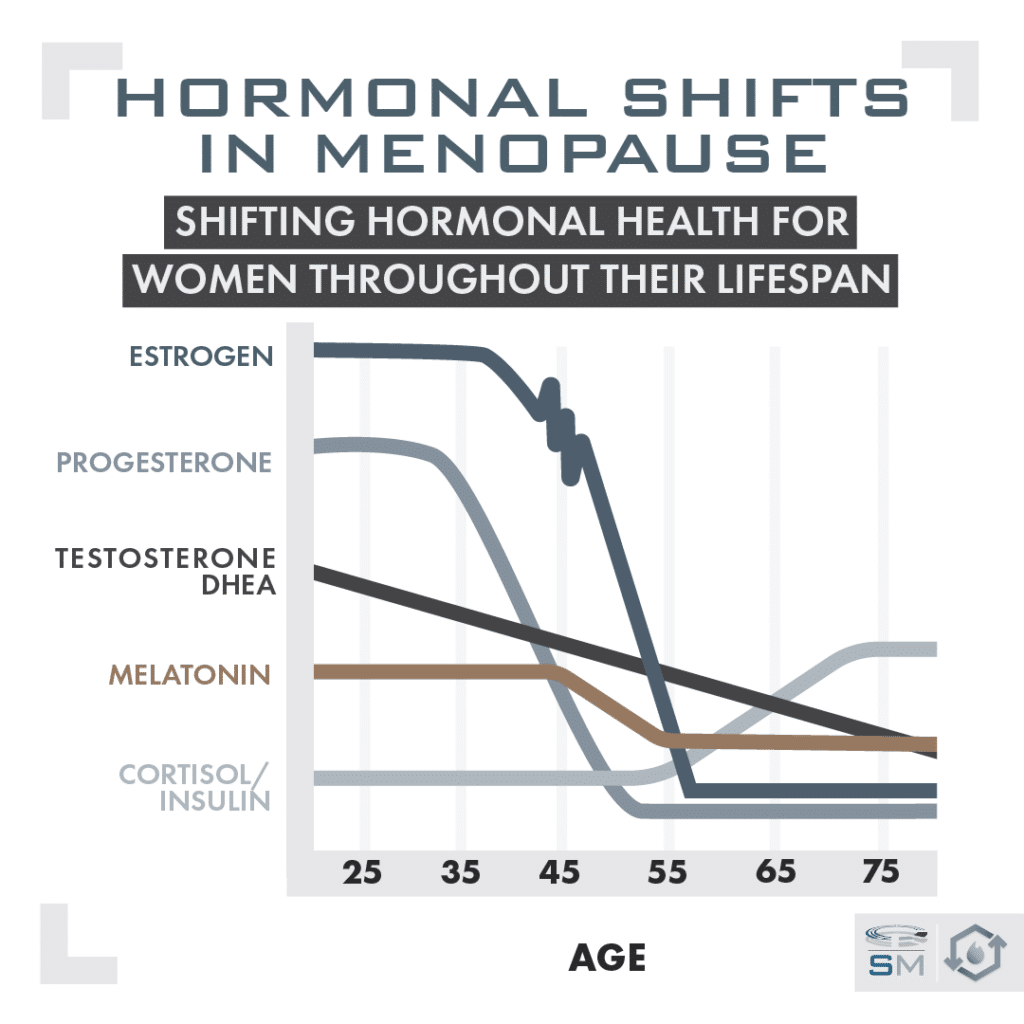
- Estrogen levels can be erratic and variable in the transitionary period, declining towards the end.
- Progesterone levels steadily decline until menopause and tend to decline first before estradiol.
- Testosterone and DHEA do not change strictly due to the menopause transition, but we do see a general decline due to age.
If you’re looking at the sex hormone panel of a client’s labs who is in their mid-40s, those are the things that might hint they’re heading towards menopause: Higher FSH and LH levels (if just FSH is high, it’s early in the transition; if both are high, it might mean the client is further into the transition). Estrogen levels could be really high or low, and progesterone levels steadily decline.
Women can have different symptoms depending on whether it is a period of high estrogen or low estrogen.
Symptoms indicating high estrogen: bloating, breast tenderness, and heavy menstrual flow.
Symptoms indicating low estrogen (and also the main symptoms post-menopause): hot flashes, night sweats, palpitations, headaches, insomnia, fatigue, bone loss, and vaginal dryness.
The swinging and variable hormones can cause depression, anxiety, and drastic mood swings as well. It’s important to note that many women will not have significant discomfort or symptoms during perimenopause, while others may experience a rollercoaster of both emotions and symptoms.
What is Postmenopause
Menopause is defined as the 12 months after the last cycle in the context of having gone through perimenopause. Meaning some women will lose their cycle for that long even if they’re not close to menopause; this will be related to too much stress, under-eating, inflammation, etc., and is much different than menopause.
Some of the changes, hormonal and otherwise, that occur in menopause both as a result of menopause but also as a result of general aging:
- Very low estrogen
- Very low progesterone
- Declining DHEA/testosterone (a consequence of age)
- Increased cortisol
- Increased insulin
- Decreased melatonin (a result of age)
- Decreased energy expenditure
Lower energy expenditure is mainly because women lose muscle mass faster with hormonal changes, which can be mitigated by building/maintaining muscle.
After menopause, women are at a higher risk of heart disease, weak bones, insulin resistance and metabolic syndrome, weight gain, and hypothyroidism compared to premenopausal women. Here’s the connection:
Estrogen has both significant cardioprotective and bone mineral density benefits, so the absence of estrogen is the main driver behind the increased risk of heart disease and osteoporosis.
Estrogen also has effects on fat storage patterns and is one of the reasons that premenopausal women tend to store more of their adipose tissue around the thigh and butt area; this changes after menopause, and women begin to store more fat around the abdomen.
Progesterone has beneficial cognitive effects in easing anxiety and also promoting memory, so we can see low progesterone may contribute to increased depression, anxiety, and brain fog post-menopause.
Important note: Postmenopausal women also tend to store more fat as visceral fat tissue, or fat around the organs in the abdominal cavity. This visceral fat storage contributes to postmenopausal insulin resistance and metabolic syndrome.

How to Help Postmenopausal Clients
It would be worth being an advocate for HRT because the benefits, with the data that we have now, seem to outweigh any risk factors. The benefits are easier fat loss and easier muscle gain with appropriate diet and training (don’t expect a miracle, but we do see small benefits here), lower risk of cardiovascular disease, lower risk of metabolic disease and insulin resistance, lower risk of autoimmune disease, and lower risk of cognitive decline.
Educate yourself on the real benefits of HRT and be able to debunk myths and concerns. Again, check out this article to do so.
Exercise to Prevent Weight Gain and Maintain Muscle
A woman approaching menopause should exercise regularly, specifically resistance training. This is one of the only ways to maintain adequate bone mineral density in the face of declining estrogen.
Ideally, the woman will have been resistance training for years prior to menopause because it’s quite hard to rebuild bone density and muscle postmenopause, but that doesn’t mean it can’t happen. Muscle is much easier to maintain, so the more muscle tissue a woman has going into menopause, the more protected she will be against metabolic syndrome/insulin resistance.
During the perimenopause transition, it’s very important to either start or keep maintaining regular exercise habits; again, mainly resistance training and as much low-grade activity, like brisk walking, as possible.
It’s even more important that women continue resistance training postmenopause.
Resistance training may help with symptoms of perimenopause, including mood swings and hot flashes. Several studies have shown a reduction in those symptoms with regular exercise.
Endurance or cardio is also good, but it shouldn’t be the sole methodology as it won’t have the same bone mineral or muscle-building benefits.
Maintain a Healthy Sleep Cycle
Many hormones and physiological processes ebb and flow throughout the day according to our circadian rhythms, and circadian rhythm disruption can result in significantly increased disease risk and lower quality of life and make it harder to transform the body.
Given the drop in melatonin as we age, it’s even more important that postmenopausal women have good circadian hygiene so they can maintain their sleep/wake rhythm.
Circadian hygiene includes:
- As much sun exposure as possible within 30 minutes to an hour of waking up (ideally 15–45 minutes) to get reset your circadian rhythm for better sleep at night.
- Eating meals during daylight hours and cutting off food intake 2–3 hours before bed. A small, healthy snack is fine if they struggle to sleep.
- Avoiding heavy exercise within a few hours before bed (ideally earlier in the day, but after work is fine if their schedule doesn’t permit).
- Sleep hygiene practices like blue light-blocking glasses at night, a cold, pitch-black sleeping environment, and cutting off electronics before bed.
This will have the effect of locking in cortisol and melatonin rhythms; meaning the individual will feel more energized in the morning, and it will be easier for them to fall asleep at night.

Maintain A Healthy Diet
Good nutrition is essential during this time, especially for women who want to maintain a healthy weight. Keeping protein high during perimenopause and postmenopause will help with satiety, energy expenditure, and building/maintaining lean body mass to keep energy expenditure higher.
Given the hormonal changes that predispose women to insulin resistance, the postmenopausal woman specifically may benefit from a slightly lower carbohydrate intake. Of course, you still have to take physical activity into account and the postmenopausal marathon runner, bodybuilder, or avid lifestyle weightlifter will need more carbohydrates than someone who has average activity levels or is just lifting 3x per week.
This can also be a case for clustering most of the starchy carbohydrate intake pre- and post-exercise for more efficient use and can also be a case for time-restricted feeding if used judiciously and intelligently.
I wouldn’t put a postmenopausal woman on a 16/8 or 20/4 intermittent fasting regimen every day; significant fasting, if overdone, has been shown to decrease blood sugar control in women (but not men) and may have other negative effects, especially if stress is high. Doing a milder time-restricted feeding protocol, like a daily 12/12 or 14/10, or doing 2-3 days a week of 16/8 may be helpful.
It may also be worth experimenting with higher intakes of soy-containing foods, ideally less processed ones, like edamame, as the phytoestrogens have been shown to help with symptoms and also may help with disease risk.
High intakes of polyphenol and antioxidant-containing vegetables should be continued for their beneficial effects on heart disease risk and metabolic syndrome risk. Specifically, we should be paying attention to food sources of magnesium, calcium for bone mineral density, selenium, zinc, all B vitamins, and vitamin K2.
Take the Right Supplements
Dietary supplements for specific to symptoms:
- DIM can be used in periods of high estrogen in perimenopause to help with estrogen detoxification, allowing more beneficial estrogen metabolites to be formed.
- St. Johns Wort, black cohosh root, red clover, and royal jelly have been shown to alleviate symptoms related to the transition, such as hot flashes and night sweats.
- Phytoestrogen has been shown to decrease symptoms in some women postmenopause, while others may not have an effect. The microbiome plays a role here as it is the bacterial metabolites of the phytoestrogens that actually have the effect.
- Glycine may help with sleep and blood sugar control
If your client decides to opt for HRT, then we won’t have to worry about the above supplements as much since the hormones will do their job in mitigating the symptoms.
Supplementation for disease risk, health, or body composition:
- Fish oil (1000 mg of both EPA and DHA) for metabolic and cardiovascular health
- Vitamin D + K2 for metabolic health, bone density, and cardiovascular health
- DHEA-S for hormonal support and potential cognitive benefits, both through perimenopause and postmenopause
- CoQ10 for cardiovascular health
- Blood sugar control supplements: Berberine HCl, Ceylon cinnamon, and/or bitter melon extract. (Berberine is probably the most effective of these three for this application.)
- Curcumin for decreasing inflammation.
- NAC can help support antioxidant status
- Ashwagandha if excess stress is present or if cortisol is high.
- If someone isn’t consuming enough of these nutrients from food, it may be helpful to supplement:
- B vitamin complex
- Magnesium
- Zinc
- Selenium
These are all considerations for your client based on what they’re experiencing from a health perspective, these aren’t blanket recommendations, nor should your client be taking ALL of these.
Pretty much all clients should at least be taking fish oil, vitamin D3, and vitamin K2, but everything else is based on your individual client’s needs.
Help Your Menopausal and Postmenopausal Clients
All that said, while it may be harder for postmenopausal clients to achieve impeccable body composition, it’s not impossible. With all of the recommendations above, you can get your postmenopausal clients great results.
References
Su HI, Freeman EW. Hormone changes associated with the menopausal transition. Minerva Ginecol. 2009 Dec;61(6):483-9. PMID: 19942836; PMCID: PMC3823936.
Molly C. Carr, The Emergence of the Metabolic Syndrome with Menopause, The Journal of Clinical Endocrinology & Metabolism, Volume 88, Issue 6, 1 June 2003, Pages 2404–2411, https://doi.org/10.1210/jc.2003-030242
Gietka-Czernel M. The thyroid gland in postmenopausal women: physiology and diseases. Prz Menopauzalny. 2017 Jun;16(2):33-37. doi: 10.5114/pm.2017.68588. Epub 2017 Jun 30. PMID: 28721126; PMCID: PMC5509968.
Taebi M, Abdolahian S, Ozgoli G, Ebadi A, Kariman N. Strategies to improve menopausal quality of life: A systematic review. J Educ Health Promot. 2018 Jul 6;7:93. doi: 10.4103/jehp.jehp_137_17. PMID: 30079364; PMCID: PMC6052783.
Fernandez ML, Murillo AG. Postmenopausal Women Have Higher HDL and Decreased Incidence of Low HDL than Premenopausal Women with Metabolic Syndrome. Healthcare (Basel). 2016 Mar 16;4(1):20. doi: 10.3390/healthcare4010020. PMID: 27417608; PMCID: PMC4934554.
Chen MN, Lin CC, Liu CF. Efficacy of phytoestrogens for menopausal symptoms: a meta-analysis and systematic review. Climacteric. 2015 Apr;18(2):260-9. doi: 10.3109/13697137.2014.966241. Epub 2014 Dec 1. PMID: 25263312; PMCID: PMC4389700.
Wang, Q., Ferreira, D.L.S., Nelson, S.M. et al. Metabolic characterization of menopause: cross-sectional and longitudinal evidence. BMC Med 16, 17 (2018). https://doi.org/10.1186/s12916-018-1008-8
Reyes FI, Winter JS, Faiman C. Pituitary-ovarian relationships preceding the menopause. I. A cross-sectional study of serum follice-stimulating hormone, luteinizing hormone, prolactin, estradiol, and progesterone levels. Am J Obstet Gynecol. 1977 Nov 1;129(5):557-64. PMID: 910845.
Schmidt PJ, Rubinow DR. Sex hormones and mood in the perimenopause. Ann N Y Acad Sci. 2009 Oct;1179:70-85. doi: 10.1111/j.1749-6632.2009.04982.x. PMID: 19906233; PMCID: PMC2891531.
Berger GM, Naidoo J, Gounden N, Gouws E. Marked hyperinsulinaemia in postmenopausal, healthy Indian (Asian) women. Diabet Med. 1995 Sep;12(9):788-95. doi: 10.1111/j.1464-5491.1995.tb02081.x. PMID: 8542739.
Jian J, Pelle E, Huang X. Iron and menopause: does increased iron affect the health of postmenopausal women? Antioxid Redox Signal. 2009 Dec;11(12):2939-43. doi: 10.1089/ars.2009.2576. PMID: 19527179; PMCID: PMC2821138.
Mehrpooya M, Rabiee S, Larki-Harchegani A, Fallahian AM, Moradi A, Ataei S, Javad MT. A comparative study on the effect of “black cohosh” and “evening primrose oil” on menopausal hot flashes. J Educ Health Promot. 2018 Mar 1;7:36. doi: 10.4103/jehp.jehp_81_17. PMID: 29619387; PMCID: PMC5868221.
Abdali K, Khajehei M, Tabatabaee HR. Effect of St John’s wort on severity, frequency, and duration of hot flashes in premenopausal, perimenopausal and postmenopausal women: a randomized, double-blind, placebo-controlled study. Menopause. 2010 Mar;17(2):326-31. doi: 10.1097/gme.0b013e3181b8e02d. PMID: 20216274.
Al-Akoum M, Maunsell E, Verreault R, Provencher L, Otis H, Dodin S. Effects of Hypericum perforatum (St. John’s wort) on hot flashes and quality of life in perimenopausal women: a randomized pilot trial. Menopause. 2009 Mar-Apr;16(2):307-14. doi: 10.1097/gme.0b013e31818572a0. PMID: 19194342.